The Science of What Happens in the Brain During a Migraine
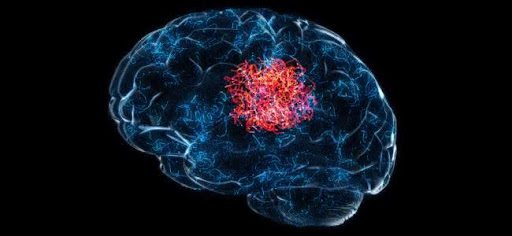
Many people get migraines and wonder why they hurt so much. A migraine is not just a bad headache; it involves complex brain changes.
This article will explain what happens in your brain during a migraine, helping you understand the pain.
Keep reading to learn more.
Key Takeaways
- Migraines move through several phases, with each phase introducing different symptoms. For example, the attack phase is when the pain hits its peak, and people might feel a throbbing pain on one side of their head.
- Triggers like stress, certain foods, or changes in the weather can kickstart a migraine by causing abnormal brain activity and chemical imbalances. This leads to heightened sensitivity to things like light and sound.
- During a migraine, blood vessels in the brain change how they behave and nerve cells become very sensitive. These changes cause intense pain.
- Some theories suggest that migraines could be due to processes such as cortical spreading depression which affects electrical activity in the brain or shifts in chemicals like serotonin and dopamine that influence how we feel pain.
- Hormones play a significant role too; for instance, changes in estrogen levels are linked to migraines in women. Understanding these hormonal influences helps tailor treatment options for menstrual migraines.
What Are the 4 Phases of a Migraine?
Migraines progress through distinct phases, including onset, hypersensitivity, attack, and aftereffects. Each phase brings its set of symptoms and challenges for those affected.
Onset
The onset stage marks the beginning of a migraine headache. Symptoms start subtly, often with warning signs like mood changes, food cravings, or a stiff neck. People with migraines might also notice increased sensitivity to light and sound, signaling that a migraine attack is approaching.
Symptoms such as mood swings and sensitivity to light can precede the severe pain characteristic of migraine attacks by several hours.
Hypersensitivity
During the hypersensitivity phase of a migraine, sufferers experience an increased reaction to external and internal stimuli. Bright lights, loud noises, or even strong smells can become unbearable.
This heightened sensitivity signals that the brain's processing of sensory information is altered. Sufferers might also notice changes in their taste or a tingling sensation on their skin.
Nerve cells in the brain become more reactive, contributing to this overwhelming sensation. For individuals going through this phase, everyday environments can turn challenging. The response to these sensations isn't just discomfort; it indicates significant changes in how migraine sufferers' brains are interpreting and responding to basic sensory inputs during a migraine episode.
Attack
The "Attack" phase marks the peak of a migraine, where individuals experience intense throbbing pain primarily on one side of their head. This severe headache can last for hours or even days, making it difficult to carry out daily activities.
Symptoms like nausea, vomiting, and extreme sensitivity to light and sound often accompany this stage. People find themselves seeking a dark, quiet place to ease their discomfort.
Changes in brain activity lead to the activation of specific nerve fibers that affect blood vessels in the brain during this period. These changes trigger the release of chemicals causing inflammation and further aggravating the headache pain.
The body's pain receptors become hypersensitive, amplifying the severity of migraine symptoms and contributing to the overall impact of the attack phase on an individual's well-being.
Aftereffect
After a migraine attack, individuals may experience what is known as the "migraine hangover." This aftereffect can bring about symptoms such as fatigue, weakness, difficulty concentrating, and even lingering head pain.
It's not uncommon for sensitivity to light and sound to persist during this time as well. These aftereffects can last for hours or even days following the initial attack.
Moving forward to "The Role of Blood Vessels and Nerve Cells"...
Migraine Relief with Botox® at Spine Team Pain Center
Experiencing 15 or more headaches a month? Botox® treatment can be a powerful tool for migraine sufferers.
Here's how it can help:
- Reduced Pain Intensity: Say goodbye to debilitating pain and regain control of your life.
- Fewer Headache Days: Enjoy more migraine-free days each month.
- Improved Quality of Life: Get back to the activities you love without worrying about migraines.
Spine Team Pain Centre can help! We offer:
- Personalized Consultations: Tailored treatment plans based on your unique needs.
- Safe and Effective Treatment: Experienced professionals ensure your comfort and well-being.
- Continued Support: We're here for you every step of the way, monitoring your progress and offering ongoing support.
Don't wait! Contact Spine Team Pain Centre today to schedule a consultation and see if Botox® treatment can be your path to migraine relief.
Related: From Pain to Relief: How Does Botox Help Migraines?
What Happens in the Brain During a Migraine?
During a migraine, external and internal triggers can cause abnormal neuron firing, chemical imbalances, and changes in nerve activity. To learn more about how these processes contribute to migraine pain, read on.
External and internal triggers
External and internal triggers play a significant role in migraine onset. These triggers can include stress, hormonal changes, certain foods or drinks, bright lights, strong smells, or weather changes.
Such triggers may lead to abnormal brain activity and chemical imbalances that can result in a migraine attack. Additionally, the brain's response to these triggers involves heightened sensitivity to stimuli and changes in nerve activity.
Understanding and avoiding these triggers is an essential part of managing migraines effectively.
Abnormal neuron firing
Abnormal neuron firing is a key factor in the development of a migraine. When triggered by external or internal factors, such as stress, hormonal changes, or certain foods, neurons in the brain's cortex can become overexcited and start firing abnormally.
This excessive neuronal activity may lead to the release of inflammatory substances and disrupt normal brain function, contributing to the throbbing pain and other symptoms experienced during a migraine attack.
Chemical imbalances within the brain can also result from abnormal neuron firing during a migraine. Changes in neurotransmitter levels, such as serotonin and dopamine, can further exacerbate neuronal hyperactivity and contribute to the persistent pain experienced by individuals with migraines.
Chemical imbalances
Chemical imbalances in the brain play a crucial role in triggering migraines. The fluctuations in serotonin, dopamine, and other neurotransmitters can lead to an increased sensitivity to pain and changes in blood vessel activity.
These imbalances can also influence how nerve cells communicate with each other, contributing to the onset of a migraine. Understanding these chemical imbalances is essential for developing targeted treatments that address the root causes of chronic migraines and provide effective relief for those experiencing debilitating symptoms.
The brain's delicate balance of chemicals like serotonin and dopamine can be disrupted by triggers such as stress, hormonal changes, or certain foods. When these chemicals are thrown off balance, it can lead to abnormal neuron firing and heightened pain responses, contributing to the development of a migraine.
Changes in nerve activity
Nerve activity changes during a migraine as neurons become hyperexcitable, firing abnormally and causing pain signals to amplify. This heightened nerve activity is often triggered by chemical imbalances in the brain.
The influx of certain neurotransmitters can contribute to the overstimulation of nerves, leading to increased sensitivity and pain perception.
Moving on to "The Role of Blood Vessels and Nerve Cells"...
How Blood Vessels and Nerve Cells Contribute to Migraines
During a migraine, blood vessels in the brain undergo changes which can lead to throbbing pain. Nerve cells become hypersensitive and play a role in the heightened sensitivity to pain.
Throbbing pain
The throbbing pain experienced during a migraine is due to changes in blood flow and increased sensitivity to pain. As blood vessels in the brain constrict and then dilate, it can result in a pulsating or throbbing sensation.
This fluctuation in blood flow triggers nerve fibers that sense pain, leading to heightened discomfort during an attack.
Changes in blood flow and increased sensitivity to pain lead to the throbbing sensation experienced during a migraine. The fluctuation of blood vessels in the brain causes them to first narrow and then expand, which activates nerve fibers responsible for sensing pain.
Changes in blood flow
Transitioning from the throbbing pain of a migraine, changes in blood flow play a crucial role in the progression of this neurological condition. As a migraine attack ensues, blood vessels in the brain constrict and then subsequently dilate, resulting in an increase in cerebral blood flow.
This alteration triggers inflammation and sensitizes nerve fibers around these arteries, contributing to the pulsating sensation experienced during a migraine episode.
During a migraine attack, alterations in blood flow can exacerbate symptoms like sensitivity to light and sound. The fluctuating blood flow may also impact certain areas of the brain responsible for processing sensory information, leading to heightened pain perception.
Sensitivity to pain
The brain's sensitivity to pain during a migraine is heightened, causing even mild stimuli to become excruciating. Pain receptors in the head and neck send signals to the brain, which amplifies the perception of pain.
This heightened sensitivity can lead to debilitating headaches and make everyday activities unbearable for those experiencing a migraine.
Role of nerve fibers
Nerve fibers play a crucial role in transmitting pain signals during a migraine. These nerves carry the pain messages from blood vessels within and around the brain to the central nervous system, intensifying sensations of throbbing or pulsating pain.
Moreover, these nerve fibers can become hypersensitive during a migraine, making individuals more susceptible to experiencing increased levels of discomfort and heightened sensitivity to light, sound, and movement.
The activation of nerve fibers also contributes to the release of certain chemicals that lead to inflammation and sensitization in the brain. As a result, this exacerbates the perception of pain during a migraine episode.
Theories Behind Migraine Pain
Theories of Migraine Pain have evolved over time, with researchers consistently exploring new avenues to explain the complex mechanisms underlying migraine headaches. Newer theories, including cortical spreading depression and chemical triggers, offer valuable insights into the multifaceted nature of migraines.
Cortical spreading depression
Cortical spreading depression is a phenomenon characterized by the temporary suppression of electrical activity in the brain's cortex. It involves a wave of depolarization followed by prolonged silencing of neurons, resulting in reduced blood flow and an altered chemical environment.
This process has been linked to the aura symptoms experienced before some migraines, such as visual disturbances and sensory changes. Researchers believe that cortical spreading depression may contribute to the initiation and progression of migraine attacks, making it a key focus in understanding the neurological mechanisms underlying migraines.
During cortical spreading depression, there is a sudden wave of neuronal excitation followed by inhibition, which can lead to changes in blood flow and trigger various migraine symptoms.
Chemical triggers
Chemical triggers play a significant role in triggering migraines. Changes in brain chemicals such as serotonin, dopamine, and calcitonin gene-related peptide (CGRP) levels can activate the pain pathways and lead to headache onset.
Serotonin levels drop during migraine attacks, affecting blood vessels and contributing to inflammation. Similarly, changes in CGRP levels can trigger the release of inflammatory substances within the brain that cause pain and hypersensitivity.
Understanding these chemical triggers is crucial for developing targeted treatments aimed at regulating their impact on migraine development and progression.
The role of estrogen
Estrogen levels naturally vary in women and are closely linked to the occurrence of migraines. Research suggests that changes in estrogen levels may trigger migraines due to their influence on brain chemicals and blood vessels.
Fluctuations in estrogen can affect how the brain responds to external triggers, leading to abnormal neuron firing and increased sensitivity to pain. The role of estrogen is particularly significant in menstrual migraines, as the drop in estrogen just before menstruation can contribute to the onset of a migraine attack.
The fluctuation of estrogen levels not only affects brain chemistry but also plays a role in altering blood vessel function, impacting nerve cells' response to pain signals. Understanding these connections between hormonal changes and migraine attacks is crucial for developing effective management strategies tailored toward addressing hormonal influences on migraine episodes while providing relief for those affected by this complex neurological condition.
Role of hormones in menstrual migraines
Hormones play a crucial role in menstrual migraines. Fluctuations in estrogen levels during the menstrual cycle can trigger migraines in some women. When estrogen levels drop before menstruation, it can lead to changes in brain chemicals and blood vessels, contributing to the onset of migraines.
Additionally, hormonal therapies such as birth control pills or hormone replacement therapy can also impact migraine frequency and severity.
Understanding the connection between hormones and migraines is essential for developing tailored treatment plans. Research shows that estrogen may not be solely responsible for menstrual migraines; other hormones like progesterone could also influence migraine patterns.
Final Thoughts on Migraine Triggers and Brain Activity
Understanding what happens in the brain during a migraine is crucial to better manage this neurological condition. External and internal triggers can set off abnormal neuron firing, leading to chemical imbalances and changes in nerve activity.
The role of blood vessels and nerve cells contributes to throbbing pain, changes in blood flow, and heightened sensitivity to pain. Several theories seek to explain migraine pain, including cortical spreading depression, chemical triggers, and the impact of hormones such as estrogen.
These insights pave the way for advanced headache management strategies tailored towards unraveling the complexities of migraines at a neurological level.
If you're struggling with migraines, consider exploring personalized treatment options. By working with a healthcare professional, you can develop a migraine management plan that addresses your specific needs.
FAQs About Migraines and Brain Activity
1. What causes migraine pain in the brain?
Migraine pain happens when certain nerves in the brain become overly sensitive and trigger a headache. This sensitivity can affect facial and scalp nerves, causing intense pain.
2. How do scientists study migraines?
Scientists use tools like functional magnetic resonance imaging (fMRI) to see what happens in our brains during a migraine. This helps them understand which parts of the brain are involved.
3. Are there different types of migraines?
Yes, there are several types of migraines, including chronic migraine and hemiplegic migraine, each with its own set of symptoms beyond just headache pain.
4. Can abdominal pain be related to migraines?
Yes, some people experience abdominal migraine, which is especially common in children. It involves similar changes in the brain that cause stomach pain instead of a headache.
5. How has our understanding of migraines changed?
Older theories about migraine pain have evolved thanks to research from organizations like the Migraine Research Foundation. Now, researchers realize that migraines involve complex changes in the brain tissue and how we feel pain.




